As an Intelligent Automation SaaS Provider, we’ve built tried and true solutions to address pain points within your business. We understand the challenge and will apply best in breed technologies to successfully apply product solutions to you enhance your internal workflow.
%20(29).jpg?width=1584&name=Newsletter%20Template%20Images%20for%20Hubspot%20(1600%20%C3%97%20900%20px)%20(29).jpg)
March 2025 Vol. 56
Welcome to this month's edition of our automation newsletter! As we navigate through an era of rapid change, the theme of "transition" resonates deeply within our industry. Healthcare providers are continually adapting to new technologies, regulations, and patient needs. Amidst these shifts, one transformative force stands out: the integration of Artificial Intelligence (AI) and Robotic Process Automation (RPA).
AI and RPA are not just buzzwords; they represent a significant transition towards more efficient, accurate, and patient-centric care. These technologies are revolutionizing how healthcare providers manage administrative tasks, streamline workflows, and enhance patient outcomes. From automating routine processes to providing advanced data analytics, AI and RPA are paving the way for a smarter, more responsive healthcare system.
In this edition, we will share how AI and RPA are already being utilized by Payors/Insurance companies and how this leaves Healthcare Providers at a disadvantage. We also share our approach to this integrated use of the two technologies, the benefits they bring, and the future possibilities they hold. Join us as we delve into the exciting world of AI and RPA and discover how these innovations are driving the transition towards a more efficient and effective healthcare landscape.
Happy reading!
CONTENT
- News
- Blog
- Payment Posting
- Products
Additional Resources
Recent Blog Posts
AI Journey 2024: Why is AI So Confusing to Understand?
Why Redundancy is Critical for an RPA/AI SaaS Company
Top Case Studies
Epic/Availity Claim Statusing Bot
Revenue Cycle Prior Authorization Case Study
We're SOC 2 Type II Certified
CampTek Software Announces SOC 2 Type II and HIPAA Compliance
%20(32).jpg)
Check out this great article: RPA to Gen AI: How AI in revenue cycle management is evolving. This is a great read, that touches upon so many important aspects of AI and the revenue cycle.
"Revenue cycle management is one of the strongest use cases for artificial intelligence in healthcare. AI in revenue cycle management has helped healthcare providers reduce claim denials and even prevent them in the first place. These solutions have also been associated with faster and more accurate data collection for claims, optimized medical coding and streamlined prior authorizations."

Developing an AI Strategy within Revenue Cycle Management
There is an ongoing war between Healthcare Providers and Payers. A majority of insurance companies are using AI to process and deny claims. Generally speaking, providers are using AI at a very limited capacity, if at all. And frankly, this puts providers and thereby their patients at a serious disadvantage. The issues are well-known: timely filing, prior/pre-authorization submission/status, medical coding discrepancies, and widespread work force challenges. Simply adding more bodies or automating the problem isn’t enough any longer. There are too many changes and variances for a provider to keep up with in Medicaid, Medicare, and commercial insurance plans.
Unlike a payor who has ONE plan to manage, a provider has MANY plans to react to and make adjustments for.
So, what can be done? The answer is AI Automation. Using this technology, one can automate the business process needed and capture data throughout the process. This data can then be leveraged to provide internal intelligence to predict, act and ensure that an authorization and/or claim is successful.
There are several steps to this approach that will ensure that not only is the process automated, but that it is done so with intelligence to gain greater success, less manual intervention, and timely filing over time. This also makes the solution more nimble and agile to adapt to the changes and variances that are inevitable with payors.
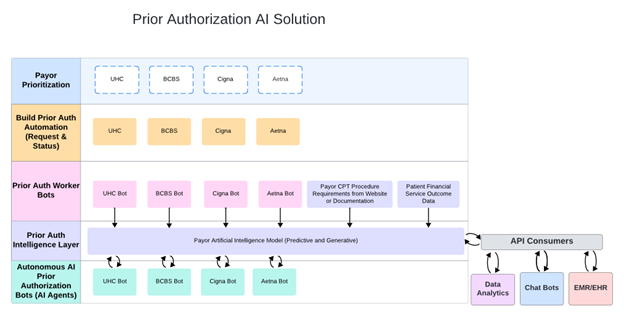
CampTek’s solution is composed of several parts:
I. Automation and AI First. Using AI, we can take a historical view of the 835 files from top payors to identify high-level trends around denials by payor, CPT code, diagnosis, physician and patient demographics.
Using this data, we build Prior Authorization Automations that perform both the request and status parts of the workflow. Our data team begins to pull the data from the automations to feed the AI Model. These automations are bespoke and will work any EMR, Payor Portal, Availity, Waystar, or other clearing houses.
See examples of the Prior Auth Request and Status Bots running in action
II. Intelligence Building. Once the automations are running in production, we begin gather data and intelligence around the authorizations that are getting statused. This data will be fed to the data model continuously. In addition, any changes in the payors plan that are communicated via their website, pdfs, or other forms are also fed to the data model to make the AI more intelligent.
III. Intelligence Consumption. This approach, in time, will provide incredible value in that it can react and adapt to payor changes, but also ensure that the prior authorization submitted will be completed and have a higher chance of acceptance. The outcome will be capturing lost top line revenue and providing specific in-house intelligence for prior authorization using predictive, generative and analytic AI intelligence. This can be consumed in a platform independent way (agentic AI Bots, data analytics programs, ChatBots, Epic or other applications that have API integration).
This is a feed and use the “brain” approach all while giving an operations team the tools it needs to be efficient, save on costs and capture the revenue that would otherwise be written off. Payers are increasingly using AI, so this is a crucial strategy for providers to have this on their roadmap, so as not to be left behind.
Overview of the Full Prior Authorization AI Solution
%20(31).jpg)
Payment Posting
Automating your Payment Posting process can be no brainer. Increasing the speed at which payments move through the revenue cycle not only increases your bottom line but also alleviates staff constraints and any back-ups that would ultimately delay your A/R cash flow.
The posting of checks is an extremely complicated but mission critical process for healthcare providers. This automated solution handles daily requirements of posting substantial amounts of payments. Timeliness is essential and the burden on the current staff can be concerning. Automating payments from the Insurance Providers can be a huge benefit for healthcare providers and help speed up AR recognition and cash flow.
This automation will work on any major EMR, Availity, Waystar and any Payor Portal. It takes 835 files in the EMR and verifies the encounter and performs validation on each of the exclusion codes. During the validation phase of this process, if there is a need to look at the PDF EOB, the bot can then extract the EOB details from Waystar and extract necessary details from PDF.
These details are also used to perform secondary adjustments, Interest Payments, multi-line payments and HRA/HSA payments. Finally, the bot confirms the payment is posted and a reconciliation report is generated. The statuses are calculated on a daily basis and provided in a spreadsheet. One of our customers needed to ramp up staff at month and quarter end to handle the larger volumes. When CampTek automated the process this staff augmentation was no longer needed.
Average Annual KPI’s:
- 75% reduction in errors causing delays
- 5000 hours saved
- 600K payments posted
- Shortened AR days and increased cash flow recognition

%20(21).jpg)
